
2025
in review
In 2025, development funding contracted globally. Yet supporters like you made it possible for us to not only maintain but grow our impact: reaching millions of people living in poverty across Africa and Asia with proven, cost-effective programs.
Some highlights from what we achieved together this year:
The communities where we work face a persistent reality: health solutions exist to save and improve lives, backed by strong evidence, but they don’t always reach the people who need them most. Our Accelerator exists to break this pattern by rigorously testing what it takes to deliver high-impact solutions at scale, and advance only those that demonstrate both strong evidence and exceptional cost-effectiveness.
In 2025, this model reached new momentum. Eight interventions progressed through late-stage testing, putting us on track for the largest wave of new program launches in Evidence Action history in 2026. In this report, you'll learn about progress on these emerging solutions alongside updates from the programs that have successfully made this journey — interventions that have been validated through rigorous testing and now operate at massive scale.
Together, these updates capture a year defined by scale, learning, and steadfast commitment to doing the most good with every dollar.




The Accelerator
Advancing evidence-based, cost-effective solutions from research to scale
The interventions progressing through our Accelerator share a common profile: strong evidence of impact in specific contexts, but no established pathway to scale. Many are overlooked within global health despite addressing persistent barriers — from poor vision to malnutrition, unsafe water, and preventable disease — that contribute to illness, missed school, and lost income.
The Accelerator is designed to close this gap. We rigorously test delivery models, assess cost-effectiveness, and advance only those interventions that can be implemented reliably, affordably, and at scale in partnership with governments.
Below are a few key developments from this year’s breakthrough Accelerator portfolio:
Reading Glasses (Uganda)
Clear vision allows adults to read, work, and maintain independence, yet millions lack access to something as simple as reading glasses. This year we provided more than 7,000 adults with glasses in Uganda while identifying models that could reliably reach those whose livelihoods depend on restored vision.
Watch: James reads from the Bible again for the first time after receiving a pair of reading glasses through an Evidence Action community distribution event
The pilot will continue into 2026 as we work to distribute a total of 25,000 pairs of eyeglasses. If results demonstrate cost-effectiveness and operational viability, we may explore expansion within Uganda or testing the model in other countries where governments support community-based vision care.
Prenatal Vitamins for Pregnant Women (Nigeria)
In 2025, we distributed 19,440 bottles of the prenatal vitamins across 90 health facilities in Nigeria. Interim analysis found that vitamin consumption increased by 60% among the women we reached, and we're now analyzing the full results to determine whether large-scale rollout in Nigeria and beyond can cost-effectively improve pregnancy outcomes for millions.
Vouchers for Water Treatment (Liberia)
Efforts to provide chlorine broadly have been vital for expanding access to safe drinking water, especially for vulnerable families. But universal access alone doesn’t guarantee use — and when households accept chlorine but don’t consistently treat their water, programs experience avoidable waste that reduces cost-effectiveness and impact. The Vouchers for Safe Water pilot tested a practical alternative: a simple voucher system that still provides chlorine for free, but only to households who actively redeem it, helping ensure the product reaches those most likely to use it.
In 2025, the pilot enrolled 9,000 pregnant women and mothers in Liberia, closely tracking redemption to understand demand and behavior. The pilot concluded in September, and endline results are now being analyzed to guide next steps and assess the model’s potential for broader scale-up.
Malaria Prevention for School-Age Children (Nigeria)
In 2025, we piloted a promising solution: providing children a full course of antimalarials at set intervals to clear existing infections and offer weeks of protection. Evidence shows this approach can reduce malaria by 40–50%, anemia by 15–23%, and may lower community transmission by 15–30%.
We delivered several cycles of treatment to school-aged children in two states in Nigeria, a country that bears 31% of global malaria deaths. Early 2026 results will assess whether this approach can be a cost-effective approach to reducing malaria transmission.
Immunization Demand Generation (Nigeria)
Millions of children continue to miss life-saving vaccines, often simply because families lack information or support. Research shows that combining simple tools like text reminders, community ambassadors, and incentives (e.g., mobile credit and coupons) can increase immunization rates by 44%. After scoping multiple countries in 2025, we have identified Nigeria — home to the world’s largest number of zero-dose children — as the highest-impact setting for a 2026 pilot.
Small Quantity Liquid Nutrient Supplements (Nigeria)
Severe acute malnutrition remains a leading cause of child death, yet there’s a proven tool to prevent it: small quantity lipid nutrient supplements (SQ-LNS) – nutrient-dense, fortified pastes in small packets designed for young children – prevent approximately 1 in 4 child deaths.
The Nigerian government secured its first large order of the supplements, and in 2025 we built strong partnerships to provide the technical support needed to ensure they reach the children most at risk. Using geostatistical modeling to target distribution, and through additional program management support, we expect to maximize the impact of the intervention to save an additional ~2,000 young lives at $1,100 per life saved* – exceptionally cost-effective even by the highest standards in global health.
*For context, GiveWell's top-rated charities typically cost $3,000-$5,500 per life saved, making this intervention roughly 2-4x more cost-effective than other highly effective programs.
At A Glance
Deworm the World
Eliminating parasitic worms as a public health problem through government-led school treatment programs
More than 895 million children globally are at-risk for parasitic worm infections, which cause anemia, malnutrition, and impaired cognitive development that lead to missed school days and reduced lifetime earnings.
Despite costing only about $0.50 per child per year to treat, many countries lack the technical capacity and resources to deliver high-quality and cost-effective mass treatment programs at scale.

Nsanje, Malawi
Nsanje, Malawi: Rose Patrick, an 11-year-old at Makoka primary school, accepts a deworming tablet during a school-based treatment event.
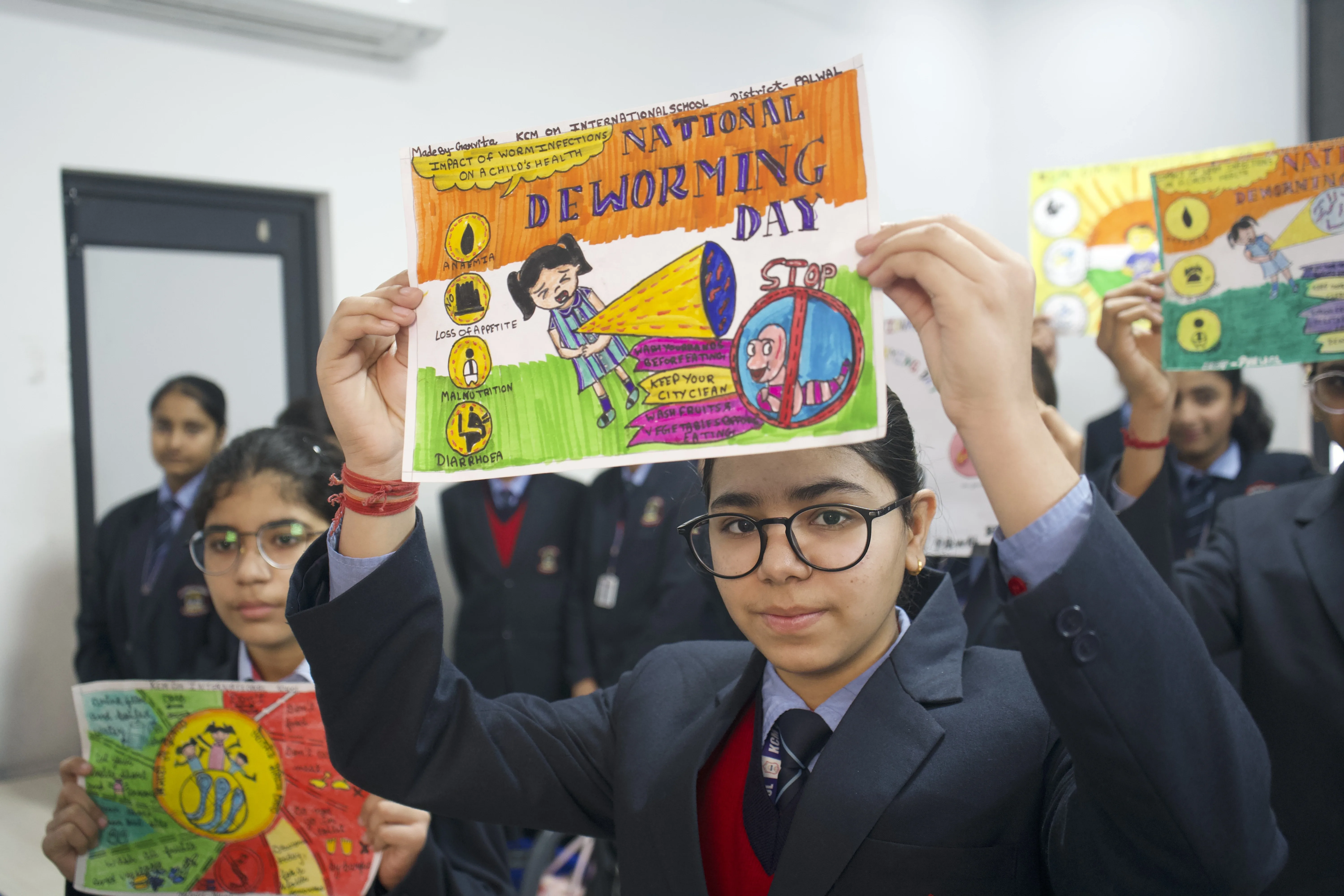
Haryana, India
Haryana, India: Garvita, a student in Haryana, India, holds up a sign she created about the effects of parasitic worm infections during a National Deworming Day event in February 2025.

Ogun, Nigeria
Ogun, Nigeria: Students gather outside of Ositelu Memorial College ahead of the Nigerian school's first deworming event.

Chikwawa, Malawi
Chikwawa, Malawi: Primary school children celebrate after a school deworming event in November 2025.

Haryana, India
Haryana, India: A child prepares to accept a deworming tablet during the National Deworming Day event in February 2025.
In 2025, we targeted 177 million children across five countries while launching a new partnership in Tanzania.
India: Strategic Government Transitions
After a decade of sustained treatment supported by Evidence Action, several Indian states have eliminated parasitic worms as a public health problem. In 2025, we scaled back or concluded our support in these states as they demonstrated the capacity to maintain programs independently.
In August 2025, National Deworming Day — one of the world's largest single-day public health campaigns — delivered treatment to 146.8 million children across the three states where we continue to provide full technical support, maintaining the massive scale we've achieved over the past decade.
We anticipate all Indian state programs will operate independently by March 2027, proving that technical assistance can be time-bound and that government systems can fully own proven interventions.
Kenya: Positioning for Complete Government Handover
Since we began supporting Kenya's national deworming program in 2012, worm infections have dropped over 80%, meaning millions of children now avoid the anemia, malnutrition, and school absenteeism these infections cause.
This progress positions Kenya to eliminate worms as a public health problem by 2027. Thanks to strong government capacity and commitment, we're now exploring our pathway to conclude our technical assistance and provide the government with the tools and resources they need to keep worm infections under control.
Nigeria: Evidence-Driven Impact Reshaping State Deworming Strategy
After seven years of partnership in Cross River State, our technical assistance helped reduce prevalence of soil-transmitted helminths by 49% and schistosomiasis (a waterborne parasitic disease) by 75%.
The recent results – collected in partnership with the Cross River state government – informed the state’s decision to reduce treatment frequency in areas where worm prevalence is now low. This approach ensures that resources are allocated more effectively and targeted to communities with the greatest need.
Pakistan: Prevalence Survey Guiding Path to Elimination
In October 2025, we launched the National Impact Survey for Pakistan’s deworming program, which we’ve supported since 2019 and now reaches about 14 million children annually. Using microscopic analysis of stool samples to measure prevalence and intensity of worms, the survey will measure the impact of the deworming rounds to inform program strategy going forwards.
At the same time, we’ve continued to work with the provincial governments to mobilize domestic resources towards the program, strengthening its long-term sustainability. As a result of these efforts, the government of Khyber Pakhtunkhwa recently made a three-year allocation to support 20% of the annual implementation budget. This represents a significant milestone and sets an important precedent for other provinces to follow.
At A Glance
Safe Water Now
Cost-effective safe drinking water through chlorine dispensers and in-line chlorination
Unsafe water causes over 1 million preventable deaths annually, with diarrheal disease ranking among the leading causes of death for children under 5. Point-of-use water treatment through chlorination can reduce under-five mortality by ~20%, yet coverage remains critically low in most low-resource settings.
In 2025, we continued reaching millions with safe water across Africa and Asia, helped shape how India defines and delivers water treatment, and made a difficult decision to reduce our dispensers footprint in Kenya while following new evidence.
India: From Pilots to National Policy
The Indian government has made a massive investment in piped water infrastructure through its Jal Jeevan Mission — expanding rural household tap connections from 32.3 million (17%) in 2019 to 157.2 million (81%) by October 2025, bringing water directly into homes that once relied on distant or unreliable sources. But infrastructure alone doesn't guarantee safe water. In 2025, our partnership helped catalyze a critical shift in focus — from building pipes to ensuring the water flowing through them is safe to drink.
Africa: Strategic Partnerships Multiply Impact
With more than 2 billion people worldwide lacking access to safe drinking water, solving this challenge requires collaborative approaches that extend beyond any single organization. In 2025, we deepened partnerships with water infrastructure providers in Malawi and Uganda as an alternate pathway to efficiently bring in-line chlorination to scale, and committed to sharing our knowledge with other organizations expanding water chlorination programs.
By working directly with organizations like Innovation: Africa and GOAL Uganda that build piped water systems in rural areas, we can layer chlorination onto existing infrastructure — ensuring communities receive safe water from the start rather than building systems from scratch. Through these partnerships in Uganda and Malawi, we brought safe water to tens of thousands more people in 2025.
Additionally, as GiveWell explores funding to other organizations to pilot water chlorination, we're sharing our operational knowledge and implementation evidence across the water treatment space. This collaborative approach means more people around the world will gain access to safe drinking water, ultimately reducing illness and deaths caused by contaminated water.
Kenya: Acting on Evidence After a Decade of Impact
When new evidence showed our dispensers program in Kenya was less cost-effective than we believed, we announced a difficult decision to reduce the scale of our programming by roughly half. Through this 18-month transition period, we’re working closely with local partners and communities to test government handover models in Busia and Siaya counties and engage communities on alternative safe water practices.
Independent monitoring revealed the program was reaching approximately 40% fewer people using treated water than our data suggested. Combined with Kenya's remarkable development over the past 12 years — GDP nearly doubled, child mortality declined over 25% — the full program no longer met our internal cost-effectiveness threshold, though it remained highly effective by standard measures.
Even as evidence required us to change course, we are proud of what our dispensers program in Kenya has achieved: 19,000 chlorine dispensers installed and safe water access extended to 2 million people each year since 2015. We estimate this intervention has prevented over 1 million cases of diarrheal disease and saved over 3,700 lives. These tangible impacts demonstrate why safe water remains a priority, even as we refocus our geographical footprint to maximize effectiveness.
At A Glance
Safe Water in Action
ASHA Health Worker
ILC Pump Operator
Community Member
Government Official
Equal Vitamin Access
Preventing anemia in children through iron and folic acid supplementation
Anemia affects children's energy, focus, and overall health, making it harder for them to learn and grow. Weekly iron and folic acid (IFA) treatments – delivered through schools and family outreach – help children stay healthier, attend school more consistently, and reach their full potential.

Chiradzulu, Malawi
Chiradzulu, Malawi: At St. Michael’s Primary School in Chiradzulu, students line up to receive iron and folic acid supplements during a routine school health distribution.

Haryana, India
School-aged girls in Haryana, India, hold out their hands to show the pink iron and folic acid tablets they take weekly to prevent anemia.

Madhya Pradesh, India
Outside their school in rural Pathrota, students smile as they hold the iron and folic acid supplements they take to prevent anemia.

Jharkhand, India
Adolescent girls take iron and folic acid supplements as part of a school-based anemia prevention effort in India.

Madhya Pradesh, India
"I have been teaching upper primary and middle classes since 1988. With IFA supplementation, we have seen a lot of improvement — children are growing healthier, more attentive, and focused in class." - Naresh Kumar Malviya, Assistant Teacher, District Narmadapuram, Madhya Pradesh
Across India and Malawi, coverage reached new highs in 2025 and demonstrated that a mix of community and school-based delivery can reach children cost-effectively and at national scale.
India: Strengthening What Works to Expand Our Impact
In 2025, we helped prevent an estimated 1 million cases of anemia across five states in India, reaching 26 million children with all recommended doses of iron and folic acid supplements. This sustains strong gains from 2022-2024 where full coverage more than doubled for both young children and school-aged children.
Throughout 2025, we worked to reach more children and make the program more sustainable. We supported states in expanding supplementation to private schools, ensuring children whose families pay for education aren't left behind. We helped governments improve supply chains so that when children show up for their weekly dose, the tablets are actually there. And we advanced strategies to improve coverage for the youngest children – those under five who don't attend school yet and rely on home visits from community health workers during their most critical developmental years.
We're now leveraging these proven strategies to expand to additional states across India. Over the two years, we anticipate roughly doubling our reach, providing millions more children with the energy to attend school, the cognitive capacity to learn and the physical strength to thrive.
Malawi: Africa's First At-Scale Proof of Concept
We successfully scaled the program to 15 districts, expanding our reach to more than 1.3 million adolescent girls. By layering iron and folic acid supplementation onto our existing deworming program, we deliver both interventions through schools using the same trained teachers and distribution systems — reaching children where they are while keeping costs low.
We focused first on adolescent girls, who face increased anemia risk with the onset of menstruation, while supporting a pilot for younger girls and boys, to demonstrate feasibility and acceptability among this age group in 2025.
With 50% of Malawi's children currently infested with worms, anemic, or both, we have a clear path to national coverage in 2026, demonstrating how this layered approach can address multiple health challenges simultaneously at scale.
At A Glance
Syphilis-Free Start
Eliminating congenital syphilis through dual HIV/syphilis rapid diagnostic tests
Congenital syphilis causes over 220,000 preventable stillbirths and newborn deaths annually, yet the solution is remarkably simple. Dual HIV/syphilis tests cost just $0.15 more than existing HIV tests and enable same-day treatment that prevents over 80% of adverse outcomes. Despite this, syphilis screening lags far behind HIV screening in most countries.
In 2025, more than 1 million pregnant women were screened for syphilis in countries where we're providing technical assistance, enabling early detection and treatment that prevented thousands of stillbirths and newborn deaths. The results we're seeing across our current footprint demonstrate that elimination is within reach — and we're building the momentum and partnerships to make it happen.
Reaching Scale Across Countries
Click on each country to explore program details and impact
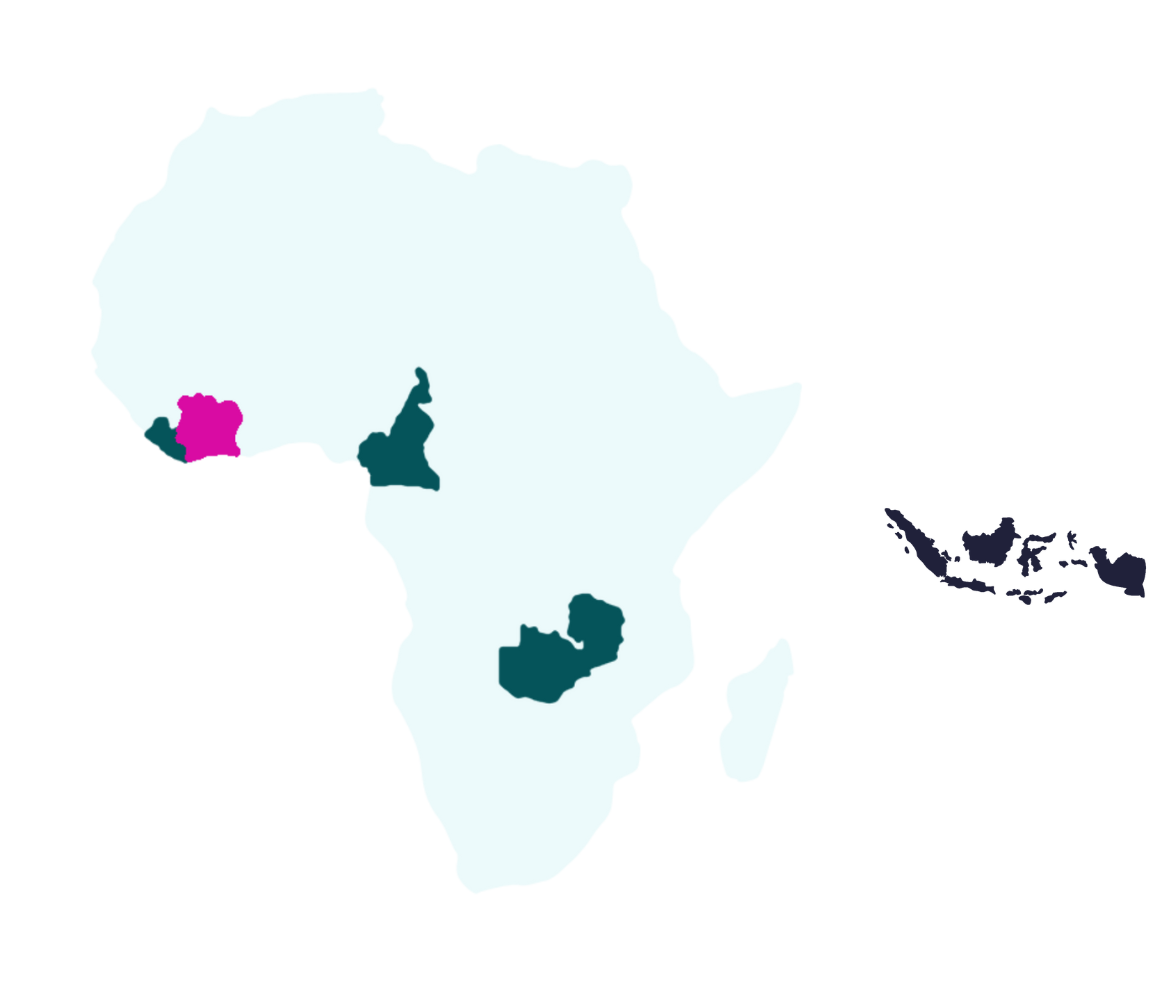
Liberia
Active ProgramCameroon
Active ProgramZambia
Active ProgramCôte d'Ivoire
New 2025Indonesia
PilotingCatalyzing a Global Movement
Evidence Action was selected from over 4,000 organizations to receive a portion of Pivotal's $250 million Action for Women's Health initiative, launched by Melinda French Gates.
At an estimated $20–$410 per DALY averted in highest-burden geographies, this ranks among the world's most cost-effective maternal health interventions — and one of the most neglected.
At A Glance
Looking Ahead to 2026
The progress shared in this report is a reflection of your continued trust in our evidence-backed approach. You make it possible for us to tackle some of global health's most neglected yet solvable problems: the reading glasses that restore livelihoods, the prenatal vitamins that prevent stillbirths, the safe water and parasite treatments that break cycles of illness and poverty.
In 2026, we're positioned to launch more programs at scale than in any year yet, continue reaching over 200 million people annually with proven interventions, and build a global coalition to eliminate the majority of the world's congenital syphilis burden. We're also experimenting with AI to learn whether it can meaningfully increase our impact.
No matter how we grow, experiment, or learn, one thing remains constant: our commitment to following the evidence to the solutions that can transform the most lives.
Thank you for making this work possible.