This story is part of our Inside the Accelerator series, which provides insight into the interventions that we’re currently exploring. Our Accelerator is our engine for new program development — it’s where we explore untapped opportunities, testing evidence-based interventions to find out which have the greatest potential for cost-effective impact and then scaling those that do.
October 2024 update: In partnership with the Nigerian government, we're now pursuing an IPTsc prevalence study and pilot in two states. While we still have some uncertainties about IPTsc, we see this pilot as a low-cost, worthwhile opportunity to explore the potential of IPTsc in malaria prevention. The prevalence study will be implemented late 2024 and the pilot will begin mid 2025.
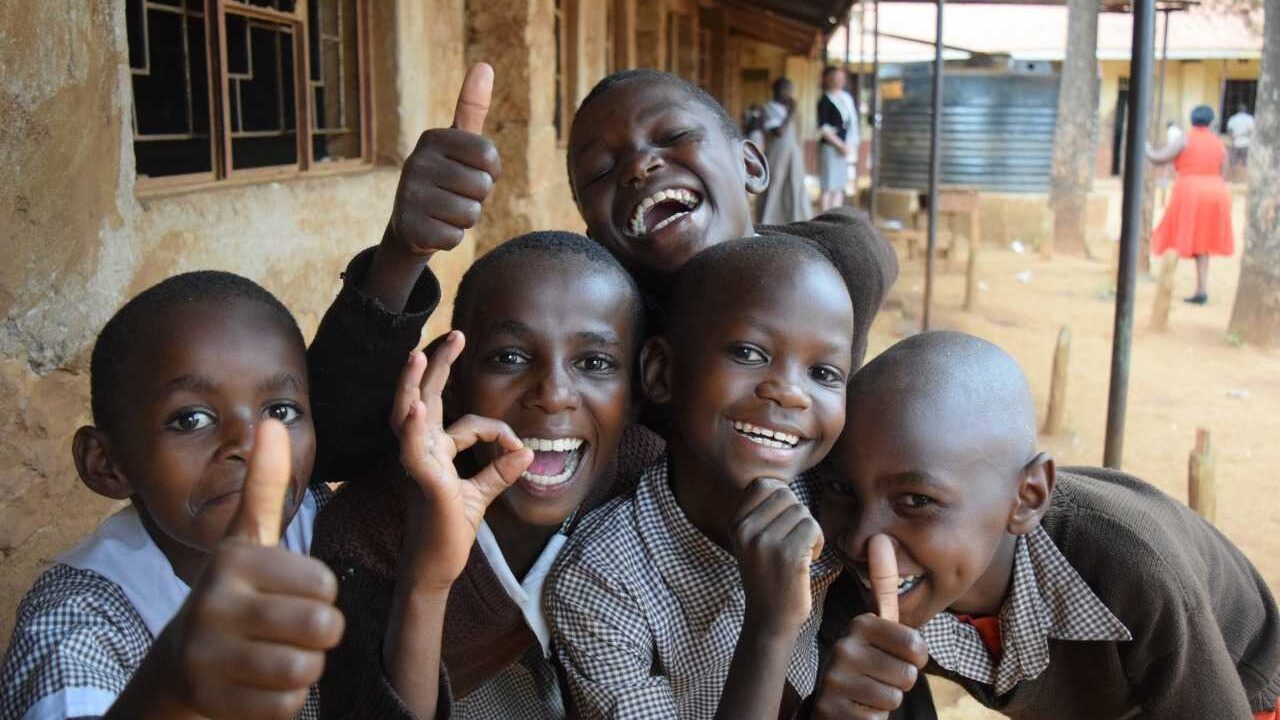
This World Malaria Day, we’re calling attention to one group that has been largely neglected in the decades-long fight against malaria: school-age children.
Most malaria prevention and treatment strategies are focused on two populations that are most vulnerable to the disease – pregnant women and children under five years old. But 200 million school-age children are also at risk for malaria, and their risk comes with severe health impacts and long-term educational and economic setbacks due to missed school days.
Research shows that school-age children may play a big role in malaria transmission. They’re carriers of the disease — meaning that many are infected with the malaria parasite, even if they’re asymptomatic, and they can transfer the parasite to mosquitos that bite them, perpetuating the cycle of infection. A range of studies have estimated the proportion of infections that school-age children drive at the community level – like this model in Uganda that indicates they may contribute to 60% of all new infections, despite comprising only 30% of the population. This data makes it all the more urgent that we turn our attention to this group if we are to reduce the global burden of malaria.
Our Accelerator is built for global health challenges like this. Our rigorous six-stage process takes a hard look at the most promising health solutions for neglected issues. We dive into evidence, test interventions in the real world, and only scale what meets our high thresholds for impact and cost-effectiveness. And when we say rigorous, we mean it — only a fraction of interventions that enter our Accelerator pipeline make it to the final stage, but those that do have our full vote of confidence.
While other organizations fighting malaria focus on pregnant women or children under five, our Accelerator team is evaluating a school-based intervention called intermittent preventive treatment of malaria in school-age children (IPTsc).
As of April 2024, IPTsc is paused in Accelerator stage 4 (scope and design). We are optimistic about its evidence-based potential in fighting malaria, but find that many questions about its cost-effectiveness are currently unanswered. And those questions are critical to understanding the bigger picture impact of IPTsc.
Evidence shows the proven power of IPTsc in combating malaria
IPTsc involves regularly providing a full course of anti-malarial drugs to school-age children regardless of their infection status. The treatment would be given to children while they’re at school — an effective delivery model that we’ve used to reach millions of children with preventative health interventions — once a school term, for three terms each year, depending on local transmission patterns. There are dual benefits – children would be simultaneously treated for malaria if they have it and protected against further infection for a period of time.
The routine provision of anti-malarial medication has been shown to help at-risk children avoid contracting the disease. Seasonal malaria chemoprevention has been implemented successfully in the Sahel region, and is so cost-effective that it’s ranked as a GiveWell top charity. But it’s specifically targeted to children under five, not school-age children – and only administered during high transmission seasons.
Our evidence review found that IPTsc is highly effective in reducing the burden of malaria.
Research indicates IPTsc can reduce the prevalence of clinical malaria – cases where patients are presenting malaria symptoms – by 50%, and parasite infection by 54%, as well as anemia by 15%. And because school-age children may act as a reservoir that perpetuates transmission, initial evidence suggests that treating them may result in a 15% community-level reduction in disease. That is very important for reducing mortality of more vulnerable groups, like children under five, who make up 80% of all malaria deaths in sub-Saharan Africa.
The WHO updated its malaria guidelines in 2022 to include IPTsc for places with moderate-to-high malaria transmission, but its latest malaria operational strategy doesn't mention it. IPTsc has yet to be implemented at scale.
Because there is no perfect solution for malaria, it’s critical that we continue to enhance our toolbox of prevention and treatment strategies – particularly as transmission patterns change through climate change and disease adaptation. The first generation of malaria vaccines targeted at infants are rolling out, and insecticide-treated bednets remain a highly cost-effective intervention. IPTsc also has the potential to be a gamechanging intervention in the global fight against malaria by targeting a historically neglected population.
But how cost-effective is implementing IPTsc at scale? That’s where we’re finding uncertainty.
More data is needed to confirm the cost-effectiveness of IPTsc
Our laser focus on cost-effectiveness is not about cutting costs – it’s about determining which interventions do the most good and maximizing the impact of each dollar invested. Assessing whether or not interventions meet our high threshold for cost-effectiveness is a pivotal part of our Accelerator process.
We modeled the estimated cost-effectiveness of IPTsc in Kenya, Uganda, Tanzania, Nigeria, and Malawi based on available data. We found it to be somewhat cost-effective in certain scenarios, but not cost-effective in others.
There are two critical program design choices that are major drivers of cost-effectiveness: drug choice and frequency of treatment. For each of these, there are no standard guidelines for implementation, so countries can choose what works best for them. Where those decisions haven’t yet been made, there’s additional uncertainty and variation in our cost-effectiveness estimates.
More importantly, there are also challenges when it comes to modeling the broader community benefits of IPTsc (in other words, the spillover effect – how much other groups, like children under five, are impacted when school-age children are treated). Unfortunately, there are limited studies on these community benefits. Because of this evidence gap, we’re still uncertain how far the impacts for the community will carry. That leaves a crucial part of our cost-effectiveness equation in limbo.
Answering these open questions may unlock the potential of IPTsc
While IPTsc is currently paused in our Accelerator — due mostly to the uncertainty around its community transmission benefits — we remain optimistic about its potential. Filling the evidence gap is critical to better understanding the impact and cost-effectiveness of this highly promising intervention that targets a neglected, but important, group. We expect new evidence that will help fill that gap to be published in the near future.
When it comes to malaria strategies, governments need to prioritize evidence and cost-effectiveness, and choose interventions that are best suited to the needs of their population. If new data shows that IPTsc meets our cost-effectiveness threshold, we’re well-positioned to translate that evidence into action. That’s what we do – we partner with governments to design and scale proven, low-cost health interventions, with long-term government ownership in mind. Our uniquely effective school-based delivery model would be well-suited for IPTsc programming – scaling through a platform that efficiently reaches school-age children, increases uptake, and lowers costs.
This year's World Malaria Day theme calls us to "accelerate the fight against malaria for a more equitable world." To build a future where malaria no longer threatens the health, education, and economic opportunities of children, we need to scale the most effective solutions that deliver outsized impact for every dollar invested.
Is IPTsc one of them? We’re waiting on new evidence to find out.